This article was originally posted in our February 2017 Newsletter, by Tom Gottschalk, COO, Medical Educator
Allied health educators are some of the most gifted people, and I feel privileged to know some of them. They are tasked to teach new inexperienced students the skills required to work in an ever-changing health care environment, often while educating seasoned employees, peers, and even the general public. Talk about hitting a moving target!
The purpose of this article is to help sharpen the saw of professionals from all areas of allied health education. It is my hope you enjoy it and find it useful for your team.
Setting the foundation
When guiding learners through new skills in education or teaching a technical task to a veteran employee, educators should know that there are three to seven levels of understanding that they have to navigate through to be considered a master in what they do. Below are three widely recognized models of this concept.
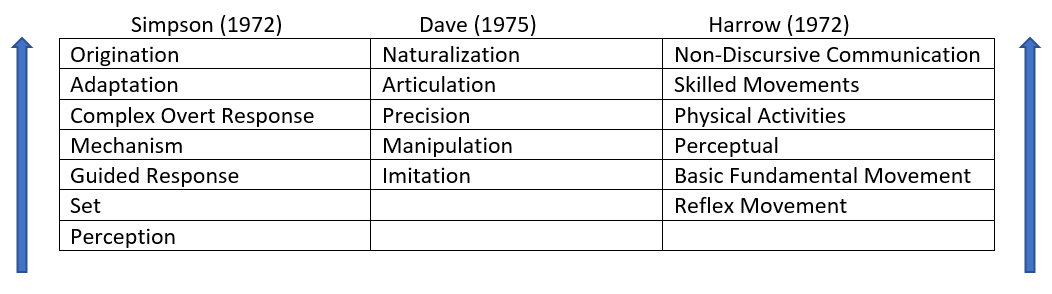
Do these terms look familiar? Where do you personally land within your area of expertise? Can you identify where your highest and lowest performing students exit your initial education program?
There are camps among us that will debate the purpose of entry level qualification testing and certification courses. Some will say they are done to assure a minimum competency is met and that the public is ultimately protected because of it. Then among the groups there are collections of experts who go one step further and say that skills evaluation should judge critical thinking and problem solving capabilities. That is a common judgement made, in my humble opinion.
So how does a program get to the higher levels of proficiency when it comes to psychomotor skills?
Below are some suggestions worth implementing to raise the bar for your students.
1. Go beyond Rote skills examinations. Stretch your students farther than just memorizing and imitating their way through dozens of one page checklists. For example, expect the learners to be able to troubleshoot and resolve predictable problems during peer reviews and teacher appraisals.
2. Run high fidelity simulations and model patient scenarios uninterrupted. i.e. Let the learners experience a close to real life experience from beginning to end without corrections. Unless the facilitator witnesses a safety concern or hazardous condition developing, there should be a “show must go on” attitude when a student is working in a contrived world. For it is in this setting the learners get a chance to enhance their critical thinking abilities and make it through a high-quality encounter that hopefully mimics the real world.
3. Form an internship program that makes a difference and is similar to a physician residency or fellowship. When their education is close to finish, release your qualified learners to a location where they can practice and perfect their chosen trade. It is here where the rubber hits the road and the apprentice get to see how they fit into their profession alongside providers who act like coaches helping them succeed. It is a true culmination that allows students to demonstrate cognitive, affective and psychomotor talents.
As 2017 rolls out in front of all us, I challenge each and every one of us to take a baby step in this direction and measure the impact. The community we serve as educators are counting on us to shape better providers to protect the public.